Asthma-COPD Overlap Syndrome (ACOS)
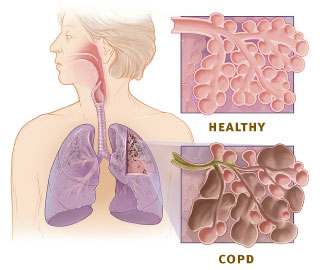
Asthma-COPD Overlap Syndrome (ACOS) is a complex respiratory condition that shares characteristics of both asthma and chronic obstructive pulmonary disease (COPD). It presents challenges in diagnosis and management, requiring a tailored approach for effective treatment.
RESPIRATORY
Rishwin A R
2/20/20252 min read
What is Asthma-COPD Overlap Syndrome (ACOS)?
ACOS is a clinical condition where individuals exhibit features of both asthma and COPD. It leads to persistent airflow limitation, chronic respiratory symptoms, and increased risk of exacerbations compared to either condition alone.
Key Characteristics:
Chronic airflow obstruction
Features of both asthma and COPD
Higher symptom burden than either disease alone
Poorer quality of life and increased healthcare utilization
Causes and Risk Factors
The exact cause of ACOS is not well understood, but several factors contribute to its development.
Common Causes:
Genetics: Family history of asthma or COPD increases susceptibility.
Environmental Exposure: Long-term exposure to pollutants, smoke, and chemicals can trigger ACOS.
Smoking: A major risk factor for COPD and a potential trigger for asthma in predisposed individuals.
Respiratory Infections: Recurrent infections in early life may contribute to airway remodeling.
Occupational Hazards: Exposure to dust, fumes, and industrial chemicals may lead to ACOS.
Symptoms of ACOS
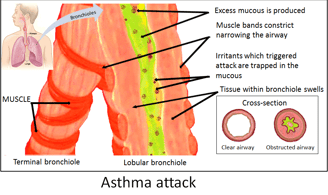
Individuals with ACOS experience symptoms that overlap between asthma and COPD, making diagnosis challenging.
Common Symptoms:
Persistent cough with or without mucus
Wheezing and shortness of breath
Frequent respiratory infections
Increased sensitivity to environmental triggers
Episodes of chest tightness
Symptoms that worsen at night or early morning
Diagnosis of ACOS
Diagnosing ACOS requires a detailed medical history, lung function tests, and clinical evaluation.
Diagnostic Approach:
Patient History: Assessment of symptoms, smoking history, and family history of respiratory diseases.
Spirometry Test: Measures airflow limitation and response to bronchodilators.
Bronchodilator Reversibility Test: Determines if lung function improves with medication, a characteristic of asthma.
Imaging Tests: Chest X-rays or CT scans to rule out other conditions.
Blood Tests: Eosinophil count and IgE levels may help differentiate asthma from COPD.
Treatment and Management
Managing ACOS requires a combination of therapies used for both asthma and COPD to improve symptoms and reduce exacerbations.
Medication-Based Treatment:
Inhaled Corticosteroids (ICS): Reduce airway inflammation (e.g., budesonide, fluticasone).
Long-Acting Beta-Agonists (LABAs): Help open airways (e.g., salmeterol, formoterol).
Long-Acting Muscarinic Antagonists (LAMAs): Improve airflow in COPD patients (e.g., tiotropium).
Combination Therapy: ICS + LABA or ICS + LAMA for optimal symptom control.
Oral Corticosteroids: Used during exacerbations to reduce inflammation.
Lifestyle Modifications:
Smoking Cessation: Essential for slowing disease progression.
Pulmonary Rehabilitation: Improves lung function and quality of life.
Regular Exercise: Enhances overall respiratory health.
Avoiding Triggers: Reducing exposure to smoke, dust, and allergens.
Vaccinations: Annual flu and pneumococcal vaccines help prevent infections.
Frequently Asked Questions (FAQs)
1. Is ACOS a separate disease?
No, ACOS is not a distinct disease but rather a combination of asthma and COPD features that require specialized management.
2. Can ACOS be cured?
There is no cure for ACOS, but proper management can control symptoms and prevent complications.
3. How is ACOS different from asthma and COPD?
ACOS includes persistent airflow limitation seen in COPD and the inflammatory, reversible airway obstruction characteristic of asthma.
4. Who is most at risk for ACOS?
Smokers, individuals with a history of asthma or COPD, and those exposed to environmental pollutants are at higher risk.
5. What is the best way to manage ACOS long-term?
A combination of medication, lifestyle changes, regular medical check-ups, and pulmonary rehabilitation is the most effective approach.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
