Acute Aortic Syndrome: Causes, Symptoms, Diagnosis, and Treatment
Acute Aortic Syndrome (AAS) is a life-threatening condition that demands immediate medical attention. Often mistaken for a heart attack due to its sudden and severe chest pain, AAS refers to a group of disorders affecting the aortic wall, including aortic dissection, intramural hematoma, and penetrating aortic ulcer. If left untreated, it can lead to catastrophic complications such as aortic rupture or organ ischemia. Understanding its causes, symptoms, and treatment options can help improve early diagnosis and patient outcomes.
VASCULAR
Rishwin A R
2/5/20253 min read
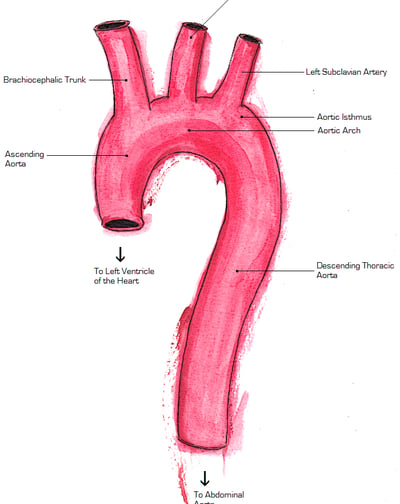
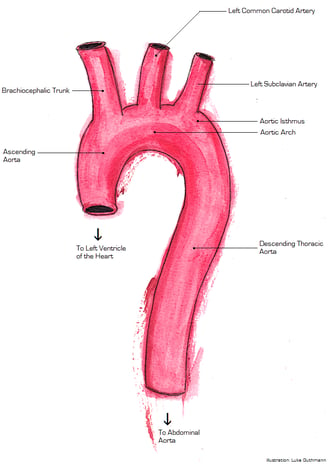
Image Credit: "Aorta Anatomy" by OpenStax College, licensed under CC BY 3.0, via Wikimedia Commons.
What is Acute Aortic Syndrome?
AAS encompasses three main conditions:
Aortic Dissection – A tear in the inner layer of the aorta, allowing blood to flow between the layers.
Intramural Hematoma (IMH) – A blood collection within the aortic wall without an obvious tear.
Penetrating Aortic Ulcer (PAU) – An ulcer-like lesion penetrating the aortic wall, potentially leading to rupture.
Each of these conditions can rapidly progress, making early intervention critical.
Causes and Risk Factors
The exact cause of AAS varies depending on the subtype, but common risk factors include:
Hypertension (High Blood Pressure) – The leading risk factor, causing excessive strain on the aortic wall.
Atherosclerosis – Plaque buildup weakens the aorta, increasing the risk of ulcers and tears.
Genetic Disorders – Conditions like Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome predispose individuals to aortic weakness.
Trauma – Blunt chest trauma, such as from a car accident, can trigger an aortic injury.
Inflammatory Conditions – Diseases like giant cell arteritis can contribute to aortic wall damage.
Cocaine or Amphetamine Use – These substances can cause sudden spikes in blood pressure, leading to aortic dissection.
Symptoms of Acute Aortic Syndrome
AAS symptoms often mimic those of other cardiac conditions, making prompt and accurate diagnosis crucial. Common symptoms include:
Sudden, severe chest pain – Often described as "tearing" or "ripping," radiating to the back.
Pain in the abdomen or lower back – Depending on the affected aortic segment.
Shortness of breath – Due to reduced blood flow to vital organs.
Sweating and pallor – Signs of shock and compromised circulation.
Loss of consciousness – A sign of critical complications like rupture or stroke.
Pulse discrepancies – Weaker pulses in one arm compared to the other.
Diagnosis
Because of its similarity to other cardiovascular emergencies, AAS requires rapid and precise diagnostic testing:
CT Angiography (CTA) – The gold standard imaging test, providing detailed visualization of the aorta.
Transesophageal Echocardiography (TEE) – A specialized ultrasound that evaluates aortic structure and function.
Magnetic Resonance Angiography (MRA) – An alternative imaging method when contrast dye is contraindicated.
Electrocardiogram (ECG) – Useful in ruling out myocardial infarction (heart attack).
Blood Tests – Checking for biomarkers such as D-dimer, which may indicate aortic dissection.
Treatment Options
Treatment depends on the severity and classification of AAS:
Medical Management
For stable patients or those with high surgical risks, conservative treatment includes:
Blood Pressure Control – Beta-blockers (e.g., esmolol, labetalol) reduce aortic stress.
Pain Management – Opioids may be used to alleviate severe pain.
Close Monitoring – Serial imaging to track disease progression.
Surgical Intervention
Emergency surgery is necessary for severe cases:
Open Aortic Repair – Involves replacing the damaged section with a synthetic graft.
Endovascular Aortic Repair (TEVAR) – A minimally invasive approach using a stent graft to reinforce the aorta.
Hybrid Procedures – Combining open and endovascular techniques for complex cases.
Prognosis and Prevention
The prognosis of AAS depends on early detection and treatment:
Without intervention, mortality rates exceed 50% within 48 hours.
Early surgical repair significantly improves survival rates.
Long-term follow-up includes regular imaging and lifestyle modifications.
Prevention Strategies
Manage Hypertension – Keep blood pressure under control with medication and lifestyle changes.
Quit Smoking – Smoking weakens the aortic wall and accelerates atherosclerosis.
Maintain a Healthy Diet – A heart-healthy diet supports vascular health.
Routine Screening for High-Risk Individuals – Those with genetic disorders or a family history of aortic disease should undergo regular imaging.
Conclusion
Acute Aortic Syndrome is a deadly but treatable condition when diagnosed promptly. Recognizing the warning signs, understanding risk factors, and seeking immediate medical care can make the difference between life and death. With advancements in imaging and surgical techniques, survival rates continue to improve. Stay informed, stay proactive, and prioritize heart health.
Frequently Asked Questions (FAQs)
1. Is Acute Aortic Syndrome the same as a heart attack?
No, AAS affects the aorta, while a heart attack results from blocked coronary arteries. However, the symptoms can be similar, making prompt diagnosis crucial.
2. How long can you survive with an untreated aortic dissection?
Survival rates drop drastically without treatment, with a 50% mortality rate within 48 hours and nearly 90% within a month.
3. Can stress cause Acute Aortic Syndrome?
Chronic stress can contribute to hypertension, a key risk factor, but it is not a direct cause.
4. What is the best imaging test for AAS?
CT Angiography (CTA) is the most effective and widely used test for diagnosing AAS.
5. Can AAS be completely cured?
While surgery or medical management can stabilize the condition, lifelong monitoring is necessary to prevent complications.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
