Asherman Syndrome: Causes, Symptoms, Diagnosis, and Treatment
Asherman Syndrome is a condition that affects the uterus, leading to scar tissue formation inside the uterine cavity. This can cause menstrual irregularities, infertility, and pregnancy complications. Though it often goes undiagnosed, timely recognition and treatment can significantly improve outcomes for affected women.
OBSTETRICS AND GYNAECOLOGY
Rishwin A R
2/2/20253 min read
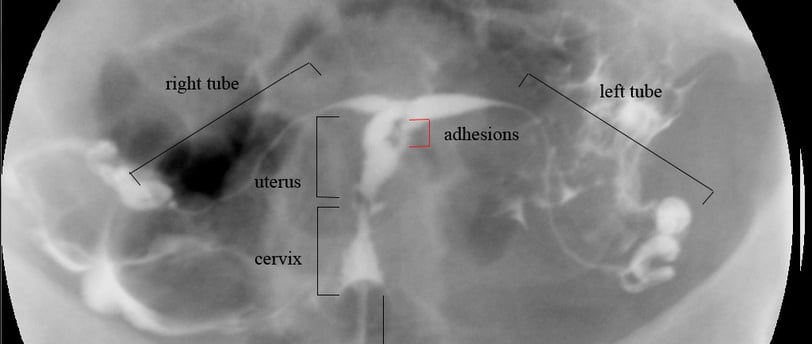
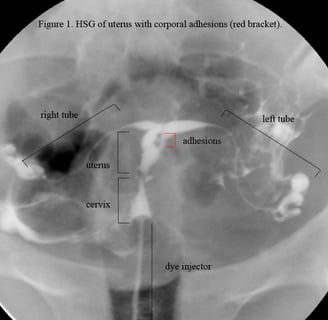
"HSG Asherman's syndrome" by Floranerolia is licensed under CC BY-SA 2.5. Source: Wikimedia Commons.
What is Asherman Syndrome?
Asherman Syndrome is characterized by the development of adhesions (scar tissue) within the uterus, which can partially or completely block the uterine cavity. These adhesions can restrict menstrual flow and affect the implantation of an embryo, making conception difficult.
Causes of Asherman Syndrome
The primary cause of Asherman Syndrome is trauma to the uterine lining, most commonly due to medical procedures. The key causes include:
Dilation and Curettage (D&C): The most common cause, often performed after a miscarriage, abortion, or excessive postpartum bleeding.
Uterine Surgery: Procedures such as myomectomy (removal of fibroids) or cesarean sections can lead to scar formation.
Infections: Severe pelvic infections, such as endometritis, can damage the uterine lining and contribute to adhesion formation.
Radiation Therapy: Rare but possible, especially in cancer treatment affecting the reproductive organs.
Diagnosis of Asherman Syndrome
Early diagnosis is crucial for effective treatment. Common diagnostic methods include:
Hysteroscopy: A thin, lighted camera is inserted into the uterus to directly visualize adhesions.
Hysterosalpingography (HSG): A specialized X-ray using contrast dye to identify blockages.
Sonohysterography: A saline-infused ultrasound that helps assess the uterine cavity.
Transvaginal Ultrasound: May suggest the presence of scarring but is less definitive than hysteroscopy.
Treatment of Asherman Syndrome
The goal of treatment is to remove adhesions and restore normal uterine function. Common treatment options include:
Surgical Treatment
Hysteroscopic Adhesiolysis: The gold standard treatment, where a surgeon carefully removes scar tissue using a hysteroscope and specialized instruments.
Balloon Stenting or IUD Placement: After surgery, a balloon or intrauterine device (IUD) may be placed to prevent reformation of adhesions.
Hormonal Therapy
Estrogen Therapy: Helps regenerate the endometrial lining after surgical intervention.
Progesterone Support: Aids in restoring normal menstrual cycles.
Post-Surgical Care
Antibiotic Treatment: If infection is suspected.
Follow-Up Hysteroscopy: Ensures that adhesions have not returned.
Lifestyle Modifications: Maintaining a healthy diet, reducing stress, and avoiding unnecessary uterine procedures can improve outcomes.
Prognosis and Fertility Outcomes
With proper treatment, many women with Asherman Syndrome can regain normal menstrual function and improve their chances of conception. However, severe cases may require advanced fertility treatments such as in-vitro fertilization (IVF) or surrogacy.
Preventing Asherman Syndrome
While not all cases can be prevented, reducing the risk involves:
Minimizing Unnecessary D&Cs: Opting for medical management of miscarriages when possible.
Ensuring Proper Postpartum Care: Prompt treatment of infections and hemorrhage.
Seeking Experienced Surgeons: For any necessary uterine procedures.
Frequently Asked Questions (FAQs)
1. Can Asherman Syndrome be completely cured?
Yes, many cases can be successfully treated with hysteroscopic surgery and post-operative care.
2. Does Asherman Syndrome always cause infertility?
Not always, but it can significantly impact fertility. Proper treatment can restore reproductive potential.
3. How long does recovery take after treatment?
Recovery varies, but most women can expect improved menstrual function within a few months post-treatment.
4. Can Asherman Syndrome come back after treatment?
Recurrence is possible, especially in severe cases. Regular follow-ups are essential to monitor progress.
5. Are there natural remedies for Asherman Syndrome?
While medical treatment is necessary, a healthy lifestyle, balanced diet, and stress management can support recovery.
Symptoms of Asherman Syndrome
Symptoms of Asherman Syndrome vary depending on the severity of adhesions but commonly include:
Light or Absent Periods (Hypomenorrhea or Amenorrhea): Due to blocked menstrual flow.
Painful Menstruation (Dysmenorrhea): Adhesions can cause cramping and discomfort.
Infertility: The condition can prevent conception or lead to recurrent miscarriages.
Recurrent Pregnancy Loss: Women with Asherman Syndrome often struggle with repeated miscarriages due to poor endometrial health.
Pelvic Pain: In severe cases, trapped menstrual blood can cause significant pain.
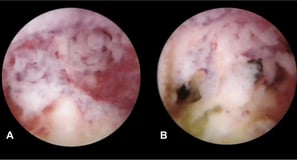
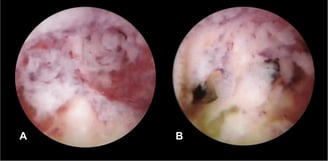
"Hysteroscopy of Asherman's Syndrome cropped" by Floranerolia, modified by Hic et nunc, is licensed under CC BY-SA 3.0. Source: Wikimedia Commons.
Adhesions in uterine wall
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
