Dressler Syndrome: Causes, Symptoms, Diagnosis, and Treatment
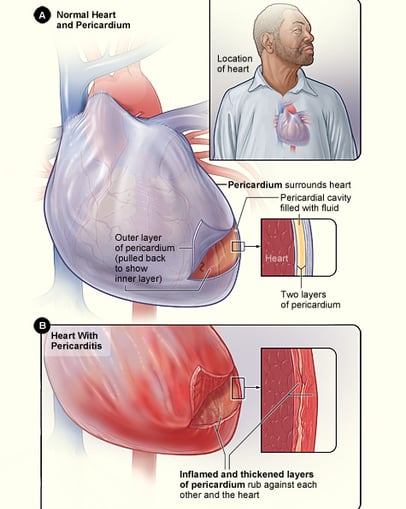
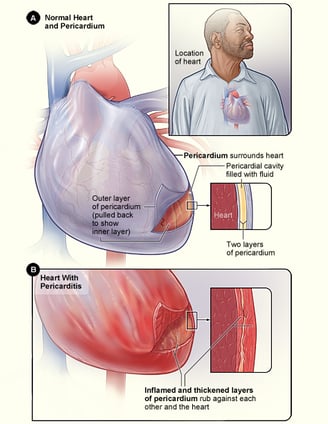
Dressler syndrome is a rare but important condition that occurs after a heart attack (myocardial infarction), heart surgery, or chest trauma. It is a type of pericarditis—an inflammation of the sac surrounding the heart (pericardium)—triggered by an immune response. While it may not be as well-known as other heart-related conditions, recognizing its signs and symptoms early can make a significant difference in treatment outcomes.
CARDIOLOGY
Rishwin A R
2/12/20253 min read
Causes of Dressler Syndrome
The exact cause of Dressler syndrome isn't fully understood, but it is believed to be an immune-mediated response. The body mistakenly attacks its own tissues following heart damage. Common triggers include:
Heart Attack (Myocardial Infarction): A major risk factor, as heart muscle damage can provoke an inflammatory response.
Heart Surgery: Procedures like coronary artery bypass grafting (CABG) or valve replacement can lead to pericardial inflammation.
Chest Trauma: Physical injury to the heart, including stab wounds or blunt force trauma, may result in an autoimmune response.
Cardiac Procedures: Interventions such as pacemaker implantation or cardiac catheterization can also trigger Dressler syndrome.
Symptoms of Dressler Syndrome
Symptoms usually develop weeks to months after a heart attack or surgery. The key symptoms include:
Chest Pain: Often sharp, worsens with deep breathing or lying down, and improves when sitting upright.
Fever: A mild-to-moderate fever is common due to inflammation.
Pericardial Friction Rub: A scratchy sound heard with a stethoscope due to pericardial inflammation.
Fatigue and Weakness: Persistent tiredness is a hallmark of many inflammatory conditions.
Shortness of Breath: May occur due to pericardial effusion (fluid buildup around the heart) or associated pleural effusion.
Joint Pain: Some patients report aching joints, similar to other autoimmune disorders.
Diagnosis of Dressler Syndrome
Early diagnosis is key to preventing complications. Physicians use a combination of clinical history, physical examination, and diagnostic tests:
1. Medical History and Physical Exam
Doctors look for a history of recent cardiac events and check for signs of pericarditis, such as chest pain that improves when leaning forward.
2. Diagnostic Tests
Electrocardiogram (ECG): May show changes consistent with pericarditis, such as widespread ST-segment elevations.
Echocardiogram: Helps detect pericardial effusion, which can indicate inflammation.
Blood Tests: Elevated inflammatory markers (C-reactive protein and erythrocyte sedimentation rate) suggest an immune response.
Chest X-ray: May show an enlarged cardiac silhouette due to fluid accumulation.


By James Heilman, MD - Own work, CC BY-SA 3.0, Wikipedia
Treatment of Dressler Syndrome
The goal of treatment is to reduce inflammation, relieve symptoms, and prevent complications. Standard treatments include:
1. Anti-Inflammatory Medications
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): First-line treatment (e.g., ibuprofen, aspirin) to reduce pain and inflammation.
Colchicine: Often added to reduce recurrence and improve treatment response.
2. Corticosteroids
Reserved for severe cases or when NSAIDs and colchicine are ineffective. Prednisone may be prescribed but is used cautiously due to potential side effects.
3. Pericardiocentesis (For Severe Cases)
If pericardial effusion leads to cardiac tamponade (a life-threatening complication where excess fluid compresses the heart), drainage may be necessary.
Complications of Dressler Syndrome
While treatment is generally effective, complications can arise if left untreated:
Chronic Pericarditis: Persistent inflammation requiring long-term management.
Pericardial Effusion: Excess fluid around the heart, which may impair its function.
Cardiac Tamponade: A medical emergency requiring immediate intervention.
Constrictive Pericarditis: Scarring and thickening of the pericardium, leading to heart dysfunction.
Prevention and Outlook
There is no guaranteed way to prevent Dressler syndrome, but early intervention and proper post-cardiac event care can reduce the risk. Colchicine has been studied as a preventive measure in high-risk individuals undergoing heart surgery.
Most cases resolve with appropriate treatment, but recurrences are possible. Patients should remain vigilant for symptoms and maintain regular follow-ups with their healthcare provider.
Frequently Asked Questions (FAQs)
1. How long does Dressler syndrome last?
The duration varies, but with treatment, symptoms typically improve within a few weeks. Some cases may last longer or recur.
2. Is Dressler syndrome life-threatening?
While not usually fatal, complications like cardiac tamponade can be dangerous. Prompt treatment is essential.
3. Can Dressler syndrome recur?
Yes, recurrence is possible, especially if not treated adequately. Colchicine is often used to prevent it.
4. Can Dressler syndrome be mistaken for a heart attack?
Yes, because it causes chest pain, it can mimic a heart attack. However, ECG and imaging help differentiate the two.
5. Is Dressler syndrome common?
It is relatively rare today due to improved post-heart attack treatments and early intervention strategies.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
