Lown-Ganong-Levine Syndrome: A Rare Heart Condition
Lown-Ganong-Levine (LGL) syndrome is a rare cardiac conduction disorder that can lead to episodes of rapid heart rate, known as tachycardia. Named after the doctors who first described it, this syndrome involves abnormalities in the electrical pathways of the heart, causing it to beat faster than normal. While rare, understanding LGL syndrome is crucial for early recognition and management.
CARDIOLOGY
Rishwin A R
12/28/20242 min read
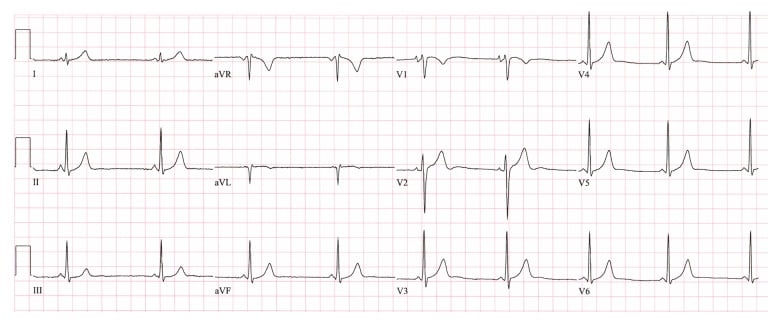
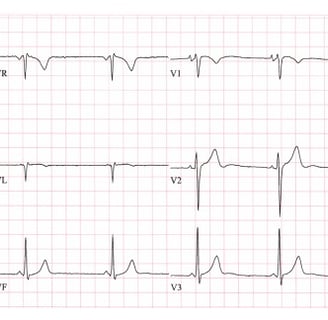
Lown-Ganong-Levine syndrome ECG by Juanita Hunter, Emmanouil Tsounias, John Cogan, and Ming-Lon Young is licensed under CC BY 4.0. Image source: Wikipedia.
What is Lown-Ganong-Levine Syndrome?
LGL syndrome is characterized by a short PR interval on an electrocardiogram (ECG) without a delta wave, often accompanied by paroxysmal supraventricular tachycardia (PSVT). This condition is linked to accessory pathways that bypass the normal conduction delay in the atrioventricular (AV) node, leading to rapid electrical conduction in the heart.
Causes
The exact cause of LGL syndrome is not fully understood, but it is believed to be associated with:
Accessory pathways: Abnormal electrical pathways in the heart, bypassing the AV node.
Genetic predisposition: Possible hereditary factors.
Structural heart anomalies: Rarely associated with structural defects in the heart.
Symptoms
Patients with LGL syndrome may experience:
Palpitations: A sensation of rapid or irregular heartbeats.
Dizziness or lightheadedness: Often caused by insufficient blood flow during tachycardia episodes.
Shortness of breath: Due to the heart’s inability to pump blood effectively.
Chest pain: Rarely, this can occur during prolonged episodes of tachycardia.
Fainting (syncope): In severe cases, due to a sudden drop in blood pressure.
Diagnosis
Diagnosing LGL syndrome involves a combination of clinical evaluation and diagnostic tests:
Electrocardiogram (ECG): Key findings include a short PR interval (<120 ms) without a delta wave.
Holter monitoring: Continuous ECG recording to detect intermittent episodes of tachycardia.
Electrophysiological studies (EPS): Used to identify accessory pathways.
Echocardiogram: To rule out structural heart disease.\
Treatment Options
Treatment for LGL syndrome aims to manage symptoms and prevent complications. Options include:
1. Lifestyle Modifications
Avoid triggers like caffeine, alcohol, and stress.
Engage in regular physical activity but avoid overexertion.
2. Medications
Beta-blockers: To control heart rate.
Calcium channel blockers: Effective in slowing conduction through the AV node.
Antiarrhythmic drugs: For patients with recurrent tachycardia.
3. Catheter Ablation
A minimally invasive procedure to destroy the accessory pathway causing abnormal conduction.
4. Emergency Management
Cardioversion: Used in acute settings for life-threatening arrhythmias.
Vagal maneuvers: Techniques like bearing down or coughing to slow heart rate during episodes.
Prognosis
LGL syndrome is generally considered benign if managed properly. However, untreated recurrent tachycardia can lead to complications such as:
Heart failure
Stroke (due to blood clots forming during prolonged tachycardia)
Sudden cardiac arrest (very rare)
Conclusion
Lown-Ganong-Levine syndrome, though rare, underscores the importance of understanding heart conduction disorders. Early diagnosis and appropriate management can significantly improve quality of life and reduce the risk of complications. If you or someone you know experiences unexplained palpitations or other symptoms, seeking medical attention is essential.
FAQs
1. Is Lown-Ganong-Levine syndrome life-threatening?
While generally benign, it can lead to serious complications if untreated, such as heart failure or stroke.
2. How is LGL syndrome different from Wolff-Parkinson-White syndrome?
LGL syndrome lacks the delta wave on ECG and involves a different accessory pathway.
3. Can LGL syndrome resolve on its own?
In some cases, symptoms may decrease with age, but medical evaluation is crucial.
4. What triggers episodes of tachycardia in LGL syndrome?
Triggers include stress, caffeine, alcohol, and certain medications.
5. Is surgery always required for LGL syndrome?
No, many cases are managed with medications or lifestyle changes. Surgery is considered for severe or recurrent symptoms.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
