MEN 2 Syndrome: A Closer Look at a Rare Condition
Imagine a condition that quietly impacts some of your body’s most vital systems. That’s what happens with Multiple Endocrine Neoplasia Type 2 (MEN 2), a rare hereditary disorder where tumors develop in glands like the thyroid, parathyroid, and adrenal glands. This condition stems from mutations in the RET proto-oncogene, making genetic testing and early intervention life-saving. While it may sound daunting, knowledge and proactive care can make a world of difference.
ENDOCRINE
Rishwin A R
12/29/20242 min read
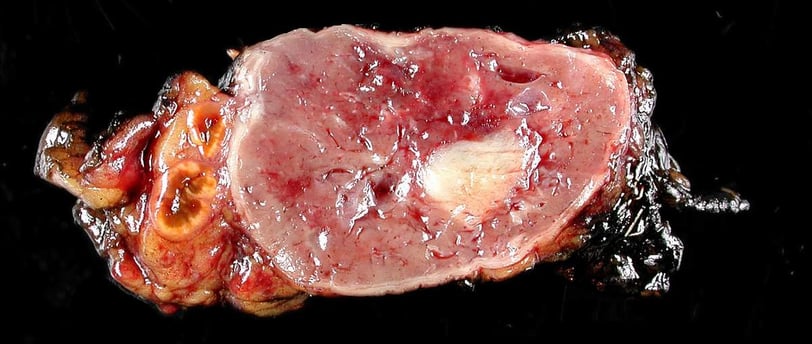
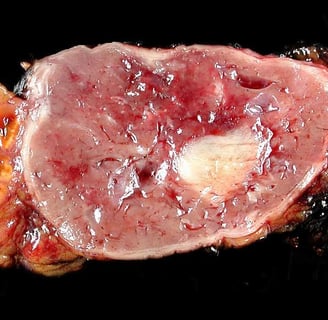
Image of adrenal paraganglioma (clinical pheochromocytoma) is used under Creative Commons Attribution-ShareAlike 3.0 Unported License. Credit: Wikipedia contributor Nephron. Source: Adrenal Paraganglioma - Clinical Pheochromocytoma
Types of MEN 2 Syndrome
MEN 2 isn’t a one-size-fits-all diagnosis; it’s divided into three distinct subtypes, each with its own personality, so to speak.
1. MEN 2A
This is the most common subtype.
It’s known for a trio of issues: medullary thyroid carcinoma (MTC), pheochromocytomas, and hyperparathyroidism.
2. MEN 2B
MEN 2B plays rougher, with more aggressive forms of MTC and pheochromocytomas.
It’s also unique in its association with physical traits like marfanoid habitus and mucosal neuromas.
3. Familial Medullary Thyroid Cancer (FMTC)
FMTC keeps things simple, focusing solely on MTC without other gland-related complications.
Causes and Risk Factors
MEN 2 isn’t something you catch; it’s something you inherit. A single genetic mutation can set the stage.
What Causes MEN 2?
The culprit is a mutation in the RET proto-oncogene, passed down in an autosomal dominant fashion. Translation? Each child of an affected parent has a 50% chance of inheriting it.
Key Risk Factors
Family history: If it runs in the family, proactive screening is non-negotiable.
Genetic predisposition: Your genes hold the key to understanding your risk.
Symptoms
MEN 2 doesn’t just whisper; it sends clear signals. Here’s what to watch for:
Thyroid-related Symptoms
A lump in your neck that doesn’t go away.
Difficulty swallowing or persistent hoarseness.
Adrenal-related Symptoms
Episodes of high blood pressure.
Sweating and rapid heartbeats (pheochromocytomas at work).
Parathyroid-related Symptoms
Kidney stones that seem to come out of nowhere.
Weak bones or unexplained bone pain.
Diagnosis
Diagnosing MEN 2 is like solving a puzzle; you need all the pieces.
Step 1: Genetic Testing
Pinpoints mutations in the RET proto-oncogene. Knowing your status changes everything.
Step 2: Biochemical Testing
Elevated calcitonin levels can reveal MTC early.
High catecholamines or metanephrines signal pheochromocytomas.
Step 3: Imaging Studies
Tools like ultrasounds and CT scans help visualize tumors before they cause trouble.
Treatment
When it comes to MEN 2, early and aggressive treatment is the name of the game.
Surgical Options
Prophylactic thyroidectomy: For those with RET mutations, removing the thyroid before cancer strikes can be lifesaving.
Adrenalectomy: Takes care of pheochromocytomas.
Medications
Supplements like calcium and vitamin D address parathyroid issues.
Targeted therapies, including tyrosine kinase inhibitors, offer hope for advanced MTC.
Complications
Left unchecked, MEN 2 doesn’t play nice. Potential complications include:
Spread of MTC to other organs.
Severe hypertension from adrenal tumors.
Kidney damage from chronic hypercalcemia.
Conclusion
MEN 2 is a condition that demands respect but not fear. With advances in genetic testing and personalized care, individuals and families affected by this syndrome can face it head-on. If there’s one takeaway, it’s this: awareness and action save lives.
FAQs
1. What is MEN 2’s most common feature?
Medullary thyroid carcinoma (MTC) tops the list in all subtypes.
2. Is MEN 2 always inherited?
Yes, it’s a genetic disorder passed down in families.
3. Can MEN 2 be completely cured?
While there’s no absolute cure, early intervention—especially surgery—can keep symptoms and complications in check.
4. How often should family members of MEN 2 patients get tested?
Regular genetic and biochemical screenings are advised, starting from childhood for at-risk individuals.
5. What’s the life expectancy for someone with MEN 2?
With timely treatment, many patients enjoy a normal life expectancy. The key is vigilance and proactive care.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
