Muckle-Wells Syndrome
Muckle-Wells Syndrome (MWS) might sound like the name of a distant place, but it’s actually a rare genetic condition that can cause a wide range of uncomfortable—and potentially serious—symptoms. Despite its rarity, understanding this condition can make a world of difference for those affected. Let’s break it down in simple terms.
GENETIC
Rishwin A R
3/10/20252 min read
What Is Muckle-Wells Syndrome?
Muckle-Wells Syndrome is a rare autoinflammatory disorder that belongs to a group of conditions known as Cryopyrin-Associated Periodic Syndromes (CAPS). It’s caused by mutations in the NLRP3 gene, which leads to excessive inflammation throughout the body.
Quick Facts:
Genetic Cause: NLRP3 gene mutation
Inheritance Pattern: Autosomal dominant
Onset: Can appear from childhood to adulthood
Prevalence: Very rare; exact numbers are unknown
Causes of Muckle-Wells Syndrome
The culprit behind Muckle-Wells Syndrome lies in the NLRP3 gene. This gene plays a key role in regulating the body’s inflammatory response. When it mutates, the immune system goes into overdrive, producing too much of an inflammatory protein called interleukin-1 beta (IL-1β).
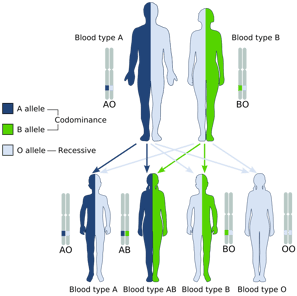
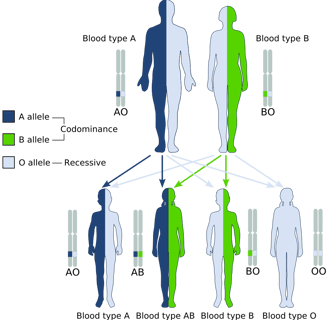
Inheritance:
Autosomal Dominant Inheritance: This means if one parent has the mutated gene, there’s a 50% chance of passing it on to their children.
Signs and Symptoms
Muckle-Wells Syndrome symptoms can vary from person to person, but here are the common ones:
Common Symptoms:
Recurrent fevers
Hives-like rash (urticarial rash)
Joint pain and swelling (arthritis)
Red, irritated eyes (conjunctivitis)
Fatigue and malaise
Serious Complications:
Progressive hearing loss
Amyloidosis (buildup of amyloid proteins in organs, especially the kidneys)
Kidney failure
How Is It Diagnosed?
Diagnosing MWS can be tricky due to its rarity and overlap with other inflammatory conditions. Here’s how doctors typically figure it out:
Diagnostic Steps:
Clinical Evaluation: Reviewing the patient’s medical history and symptoms
Genetic Testing: Identifying mutations in the NLRP3 gene
Lab Tests: Checking inflammatory markers like C-reactive protein (CRP) and serum amyloid A (SAA)
Treatment Options
While there’s no outright cure for Muckle-Wells Syndrome, modern treatments can manage symptoms and prevent complications.
Medications:
IL-1 inhibitors: These medications block the action of interleukin-1, reducing inflammation. Common options include:
Anakinra
Canakinumab
Rilonacept
Supportive Care:
Hearing aids for hearing loss
Kidney monitoring to catch any early signs of damage
Regular follow-ups to adjust treatments as needed
FAQs About Muckle-Wells Syndrome
1. Is Muckle-Wells Syndrome contagious?
No, it’s a genetic condition and cannot be passed from person to person like an infection.
2. Can MWS be cured?
Currently, there’s no cure, but IL-1 inhibitors can control symptoms effectively.
3. What’s the life expectancy for someone with MWS?
With proper treatment, life expectancy can be normal, though complications like amyloidosis can pose risks if not managed.
4. How common is Muckle-Wells Syndrome?
It’s extremely rare, and the exact number of cases worldwide isn’t known.
5. Are children at risk if a parent has MWS?
Yes, there’s a 50% chance of passing the mutated gene to a child if one parent has MWS.
Example of a genetic condition passing down the generation
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
