Neuroleptic Malignant Syndrome (NMS): A Life-Threatening Reaction to Antipsychotics
Neuroleptic Malignant Syndrome (NMS) is a rare but potentially fatal reaction to antipsychotic medications. It is characterized by a dangerous combination of high fever, muscle rigidity, altered mental status, and autonomic dysfunction. Though uncommon, its severity makes early recognition and treatment crucial. In this article, we'll explore the causes, symptoms, diagnosis, and treatment of NMS.
NEUROLOGY
Rishwin A R
2/9/20252 min read
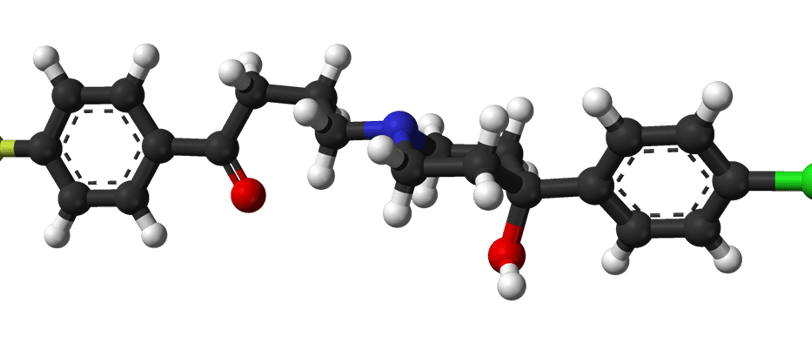
Structure of Haloperidol
Causes and Risk Factors
NMS is primarily triggered by dopamine-blocking agents, mainly antipsychotic drugs. The exact mechanism isn't fully understood, but the primary culprit is dopamine receptor blockade in the brain, particularly in the hypothalamus.
Common Triggers
First-generation (typical) antipsychotics – Haloperidol, Chlorpromazine, Fluphenazine
Second-generation (atypical) antipsychotics – Risperidone, Olanzapine, Clozapine
Other dopamine antagonists – Metoclopramide, Promethazine
Abrupt withdrawal of dopamine agonists – Seen in Parkinson’s disease patients suddenly stopping medications like Levodopa
Risk Factors
High doses or rapid dose escalation of antipsychotics
Dehydration and electrolyte imbalances
Previous history of NMS
Underlying neurological disorders (e.g., Parkinson’s disease)
Male gender and younger age – More commonly seen in men under 40
Symptoms: Recognizing the Warning Signs
NMS presents with a distinctive set of symptoms that develop over hours to days. The classic tetrad includes:
1. Hyperthermia (High Fever)
Body temperature often exceeds 38.5°C (101.3°F), sometimes reaching dangerous levels (>40°C).
2. Muscle Rigidity
"Lead-pipe" rigidity, meaning the muscles remain stiff and resistant to passive movement.
Can cause rhabdomyolysis (muscle breakdown), leading to kidney damage.
3. Altered Mental Status
Confusion, agitation, delirium, or even coma.
4. Autonomic Dysfunction
Fluctuating blood pressure
Excessive sweating (diaphoresis)
Irregular heart rate (tachycardia)
Difficulty breathing
Diagnosis: How is NMS Identified?
There is no single test to confirm NMS, making clinical judgment essential. However, doctors use a combination of symptoms, history, and laboratory findings to diagnose it.
Key Diagnostic Criteria
Recent use of dopamine-blocking medications
High fever and muscle rigidity
Elevated creatine kinase (CK) levels – A marker of muscle breakdown
Leukocytosis (high white blood cell count)
Electrolyte imbalances (e.g., low sodium)
Differentiating from Similar Conditions
Serotonin Syndrome – Features hyperreflexia and clonus (jerky movements), whereas NMS causes rigid muscles.
Malignant Hyperthermia – Occurs after anesthesia, not antipsychotic use.
Severe infections (sepsis) – Must be ruled out through blood tests and cultures.
Treatment: A Race Against Time
Early intervention is key to preventing complications. The mainstay of treatment is stopping the offending drug and providing supportive care.
1. Immediate Discontinuation of Antipsychotics
The first and most critical step.
2. Supportive Care
Cooling measures – Ice packs, cooling blankets, IV fluids to manage hyperthermia.
IV hydration – Prevents kidney damage from muscle breakdown.
Electrolyte correction – Addresses sodium, potassium, and other imbalances.
3. Medications to Reverse Symptoms
Dantrolene – A muscle relaxant that reduces rigidity and fever.
Bromocriptine – A dopamine agonist that counteracts dopamine blockade.
Benzodiazepines (e.g., Lorazepam, Diazepam) – Helps control agitation and seizures.
4. Intensive Care Monitoring
Severe cases may require ICU admission for mechanical ventilation and cardiac monitoring.
Prevention: Can NMS Be Avoided?
While NMS cannot always be predicted, certain strategies can reduce the risk:
Start antipsychotics at low doses and increase gradually.
Monitor patients closely for early signs, especially after dose changes.
Ensure proper hydration and avoid excessive heat exposure.
Use alternative medications in high-risk patients.
Educate patients and caregivers about warning signs.
FAQs
1. Is NMS reversible?
Yes, with prompt treatment, most patients recover fully within 1-2 weeks.
2. Can NMS recur?
Unfortunately, yes. Patients who have had NMS before are at higher risk if re-exposed to antipsychotics.
3. How common is NMS?
It is rare, affecting approximately 0.02% to 3% of individuals on antipsychotic medications.
4. Does NMS only occur with high doses of antipsychotics?
No, it can happen at any dose, but higher doses and rapid increases raise the risk.
5. How is NMS treated?
The primary treatment is stopping the offending medication immediately and providing supportive care, including IV fluids, cooling measures, and medications like dantrolene or bromocriptine to help reverse symptoms.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
