Parinaud Syndrome
Parinaud Syndrome, also known as Dorsal Midbrain Syndrome, is a rare neurological condition affecting eye movement and pupil function. Named after French ophthalmologist Henri Parinaud, this disorder typically results from damage to the upper brainstem. Although uncommon, understanding this syndrome is crucial because its signs can often indicate serious underlying conditions.
OPTHAMOLOGYNEUROLOGY
Rishwin A R
3/14/20252 min read
What is Parinaud Syndrome?
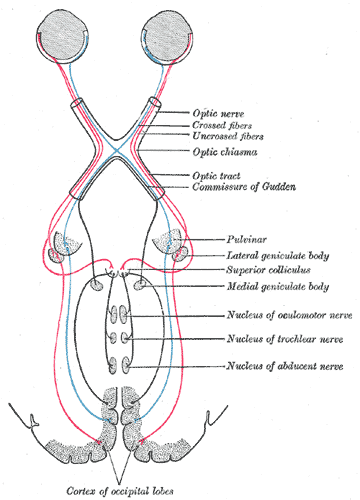
Parinaud Syndrome refers to a group of eye movement abnormalities due to damage in the dorsal midbrain, particularly the pretectal region. This area controls vertical eye movements and pupil reactions.
Key Points:
Also called Dorsal Midbrain Syndrome.
Affects vertical gaze, especially upward eye movements.
Typically results from compression or lesions in the midbrain.
Causes of Parinaud Syndrome
Several conditions can lead to Parinaud Syndrome by affecting the dorsal midbrain:
1. Pineal Gland Tumors
These tumors can press on the midbrain.
Common in young adults and adolescents.
2. Multiple Sclerosis (MS)
MS lesions can damage the brainstem.
3. Stroke (Brainstem Infarct)
Disruption of blood flow causes brainstem damage.
4. Hydrocephalus
Increased intracranial pressure affects the midbrain.
5. Trauma
Direct injury to the brainstem.
Symptoms of Parinaud Syndrome
The symptoms are mostly related to eye movement and visual control but can sometimes involve other neurological issues.
1. Upward Gaze Palsy
Difficulty or inability to move the eyes upward.
2. Convergence-Retraction Nystagmus
Eyes jerk back into the socket when attempting to look up.
3. Light-Near Dissociation
Pupils react to near objects but not to light.
4. Eyelid Retraction (Collier’s Sign)
Upper eyelids appear wide open, giving a startled look.
5. Diplopia (Double Vision)
May occur due to impaired eye movement.
6. Other Neurological Signs
If the midbrain damage is extensive, there may be additional symptoms like headaches, nausea, and imbalance.
Diagnosis of Parinaud Syndrome
A detailed neurological examination is essential. Eye movement tests are often the first clue.
Diagnostic Steps:
Clinical History and Examination
Focus on eye movements and pupil response.
Neuroimaging
MRI or CT scans to detect midbrain lesions, tumors, or hydrocephalus.
Lumbar Puncture (if needed)
To check for increased intracranial pressure or infection.
Treatment of Parinaud Syndrome
Treatment focuses on addressing the underlying cause. The syndrome’s eye movement issues may improve once the primary problem is treated.
1. Tumor Management
Surgical removal, radiation, or chemotherapy for pineal tumors.
2. Treating Hydrocephalus
Ventriculoperitoneal (VP) shunt to drain excess fluid.
3. Managing Multiple Sclerosis
Steroids or immunomodulatory therapy.
4. Stroke Rehabilitation
Focus on physical therapy and neurological support.
Symptomatic Relief:
Prism glasses for double vision.
Occupational therapy for visual impairments.
Prognosis
The outlook depends on the underlying cause and the severity of midbrain damage.
Early diagnosis and treatment improve outcomes.
Some eye movement problems may be permanent, but many patients adapt well.
Frequently Asked Questions (FAQs)
1. Is Parinaud Syndrome permanent?
Some symptoms, especially eye movement issues, may persist, but outcomes vary depending on the underlying cause and treatment.
2. Can Parinaud Syndrome be the first sign of a brain tumor?
Yes. Pineal tumors often present first with Parinaud symptoms due to midbrain compression.
3. Is there a cure for Parinaud Syndrome?
There's no universal cure. Treatment targets the underlying cause, which may alleviate the syndrome.
4. What is Collier’s Sign?
It’s an abnormal eyelid retraction where the upper lids are higher than normal, creating a wide-eyed appearance.
5. How is Parinaud Syndrome different from other eye movement disorders?
It specifically involves vertical gaze palsy, usually upward gaze, and unique features like light-near dissociation and convergence-retraction nystagmus.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
