Red Man Syndrome
Red Man Syndrome (RMS) is a non-allergic reaction caused by the rapid infusion of vancomycin, leading to histamine release. It results in flushing, itching, low blood pressure, and rapid heart rate, primarily affecting the face, neck, and upper body. While alarming, RMS is preventable and manageable with proper infusion techniques and premedication.
IATROGENIC
Rishwin A R
2/20/20252 min read


What is Red Man Syndrome?
Red Man Syndrome is a non-allergic infusion reaction that occurs due to the rapid administration of vancomycin. Unlike true allergic reactions, RMS is a histamine-mediated response, meaning it results from the body's immune cells releasing histamine rather than an antibody-driven immune attack.
Causes of Red Man Syndrome
The primary cause of RMS is the rapid infusion of vancomycin, which leads to excessive histamine release. Other contributing factors include:
Higher doses of vancomycin
Pre-existing mast cell disorders
Administration without premedication (e.g., antihistamines)
Symptoms of Red Man Syndrome
Symptoms typically begin within 10–30 minutes of starting the infusion, although they can appear later. Common signs include:
Flushing and redness of the face, neck, and upper body
Itching (pruritus), sometimes intense
Low blood pressure (hypotension)
Dizziness or lightheadedness
Rapid heart rate (tachycardia)
Swelling of the face or upper torso (in rare cases)
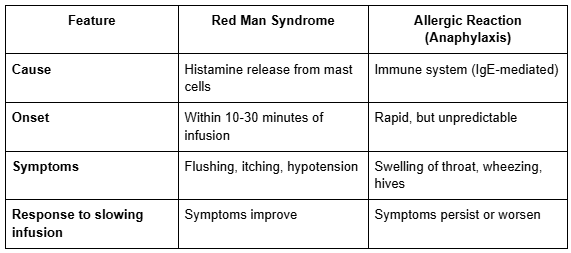
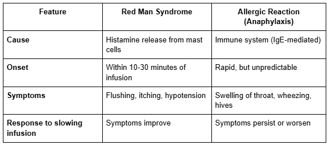
Differentiating RMS from an Allergic Reaction
A common concern is distinguishing RMS from a true allergic reaction. Key differences include:
Diagnosis of Red Man Syndrome
Diagnosis is clinical, based on the patient's symptoms and history of vancomycin administration. There are no specific lab tests for RMS, but healthcare providers may check for:
Histamine levels in blood (in research settings)
Skin testing to rule out true allergy
Treatment and Management
Immediate Steps
If RMS occurs during an infusion, the following steps should be taken:
Stop or slow down the vancomycin infusion immediately
Administer antihistamines, such as diphenhydramine (Benadryl), to counteract the histamine release
Provide IV fluids if the patient experiences low blood pressure
Monitor vital signs closely
Prevention Strategies
To reduce the risk of RMS in patients receiving vancomycin:
Infuse vancomycin slowly over at least 60 minutes (or even longer for higher doses)
Premedicate with antihistamines if the patient is at risk
Consider alternative antibiotics in high-risk cases
Conclusion
Red Man Syndrome is an unsettling but preventable reaction to vancomycin infusion. By understanding its causes, symptoms, and management, healthcare professionals can ensure patient safety while still using this powerful antibiotic. If you've ever experienced RMS, knowing that it’s a temporary, treatable condition can ease concerns the next time vancomycin is required.
FAQs
1. Is Red Man Syndrome dangerous?
While it can be uncomfortable and alarming, RMS is not typically life-threatening and resolves with proper management.
2. Can RMS occur with other antibiotics?
Though vancomycin is the primary culprit, similar reactions have been reported with rifampin and certain other drugs that trigger histamine release.
3. How long does Red Man Syndrome last?
Most symptoms resolve within a few hours once the infusion is stopped or slowed and antihistamines are given.
4. Can I take vancomycin again if I’ve had RMS before?
Yes, but it should be given slowly and possibly with premedication to prevent recurrence.
5. What’s the difference between Red Man Syndrome and an allergy to vancomycin?
RMS is a histamine reaction, while a true allergy involves the immune system and can be life-threatening. RMS improves when the infusion is slowed, whereas an allergy requires complete avoidance of vancomycin.
Syndromes.xyz
Explore medical syndromes and their details here.
For Educational purposes only
The information on this site is not in any way, replacement for professional advice. Always consult your physician regarding personal queries
Connect
Support
syndromesxyz@gmail.com
© 2024. All rights reserved.
